Article Summary
This comprehensive guide examines the F12.20 ICD-10 code, which represents Cannabis use disorder with intoxication. Healthcare providers need accurate documentation and proper code application to achieve optimal reimbursement rates.
The article covers diagnostic criteria, clinical applications, documentation requirements, and billing procedures for the F12.20 code. Additionally, this guide explores related mental health and cardiology CPT codes that frequently accompany F12.20 in patient care scenarios.
What is F12.20 ICD-10 Code?
The F12.20 ICD-10 code specifically identifies Cannabis use disorder with intoxication, unspecified. This diagnostic code falls under the broader category of Mental, Behavioral, and Neurodevelopmental disorders (F01-F99) in the ICD-10-CM classification system. Medical professionals use F12.20 when documenting cases where patients exhibit both cannabis use disorder symptoms and current intoxication effects.

Healthcare providers must recognize that F12.20 requires specific clinical documentation to support proper code assignment. The code applies when patients present with problematic cannabis use patterns combined with active intoxication symptoms at the time of evaluation.
Clinical Criteria for F12.20 Code Assignment
Proper F12.20 code application requires medical professionals to identify specific clinical presentations. The diagnostic criteria encompass both cannabis use disorder symptoms and concurrent intoxication manifestations.
| Clinical Component | Required Documentation | Coding Impact |
| Cannabis Use Pattern | Problematic use causing significant impairment | Primary diagnosis requirement |
| Intoxication Symptoms | Active cannabis effects present during evaluation | Modifier specification |
| Timeline Documentation | Current episode with intoxication | Code accuracy validation |
| Severity Assessment | Mild, moderate, or severe classification | Additional coding consideration |
Medical professionals should document the presence of cannabis intoxication symptoms such as impaired coordination, altered perception, or cognitive changes. These symptoms must be present during the clinical encounter to justify F12.20 code assignment.
Documentation Requirements for F12.20
Accurate F12.20 documentation requires comprehensive clinical notes that support both the cannabis use disorder diagnosis and the current intoxication state. Healthcare providers must record specific observations and patient-reported symptoms.
| Documentation Element | Required Details | Purpose |
| Substance Use History | Frequency, duration, amount consumed | Establishes disorder pattern |
| Current Symptoms | Active intoxication signs observed | Justifies F12.20 vs F12.10 |
| Functional Impairment | Work, social, or personal impact | Supports disorder criteria |
| Physical Examination | Vital signs, neurological findings | Medical necessity evidence |
| Mental Status Exam | Cognitive function, mood assessment | Comprehensive evaluation |
Clinical documentation must clearly distinguish between cannabis use disorder with intoxication (F12.20) and without intoxication. This distinction affects both medical decision-making and reimbursement outcomes.
Billing Procedures for F12.20
Medical billing for F12.20 requires attention to specific payer requirements and documentation standards. Insurance companies scrutinize substance use disorder claims, making accurate documentation critical for successful reimbursement.
The F12.20 code often pairs with specific CPT codes for mental health services. Common combinations include evaluation and management codes for psychiatric services and psychotherapy sessions that address cannabis use disorders.
| Billing Component | Requirements | Common Issues |
| Primary Diagnosis | F12.20 as principal diagnosis | Incorrect code selection |
| Supporting CPT Codes | Mental health service codes | Missing procedure documentation |
| Medical Necessity | Clear clinical justification | Insufficient documentation |
| Payer Guidelines | Insurance-specific requirements | Claim denials |
Healthcare providers should verify payer-specific requirements for F12.20 claims before submission. Some insurers require pre-authorization for substance use disorder treatments, which can affect claim processing timelines.
Professional medical billing services can help navigate the complexities of F12.20 coding and reimbursement. MCB’s revenue cycle management services specialize in mental health billing procedures and can optimize F12.20 claim outcomes.
Related Mental Health ICD-10 Codes
The F12.20 code exists within a broader framework of substance use disorder classifications. Healthcare providers frequently encounter related codes when treating patients with complex mental health presentations.
| ICD-10 Code | Description | Clinical Relationship |
| F32.1 | Major depressive disorder, single episode, moderate | Common comorbidity |
| F32.2 | Major depressive disorder, single episode, severe without psychotic features | Concurrent diagnosis |
| F41.1 | Generalized anxiety disorder | Frequent co-occurrence |
| F43.10 | Post-traumatic stress disorder, unspecified | Related substance use |
| F84.0 | Autistic disorder | Special population consideration |
Mental health professionals often document multiple diagnoses when treating cannabis use disorders. The comprehensive list of mental health ICD-10 codes provides additional context for complex cases involving F12.20.
CPT Codes for Mental Health Services with F12.20
Healthcare providers use specific CPT codes when delivering mental health services to patients with F12.20 diagnoses. These procedure codes determine reimbursement rates and must align with documented services.
| CPT Code | Service Description | Typical Duration | Reimbursement Considerations |
| 90791 | Psychiatric diagnostic evaluation | 60-90 minutes | Initial assessment code |
| 90834 | Psychotherapy, 45 minutes | 38-52 minutes | Standard therapy session |
| 90837 | Psychotherapy, 60 minutes | 53+ minutes | Extended therapy session |
| 90846 | Family therapy without patient | 50 minutes | Family involvement |
| 90853 | Group psychotherapy | Variable duration | Cost-effective treatment |
The combination of F12.20 with appropriate mental health CPT codes creates comprehensive billing scenarios that reflect the full scope of patient care. Proper code pairing maximizes reimbursement while maintaining compliance standards.

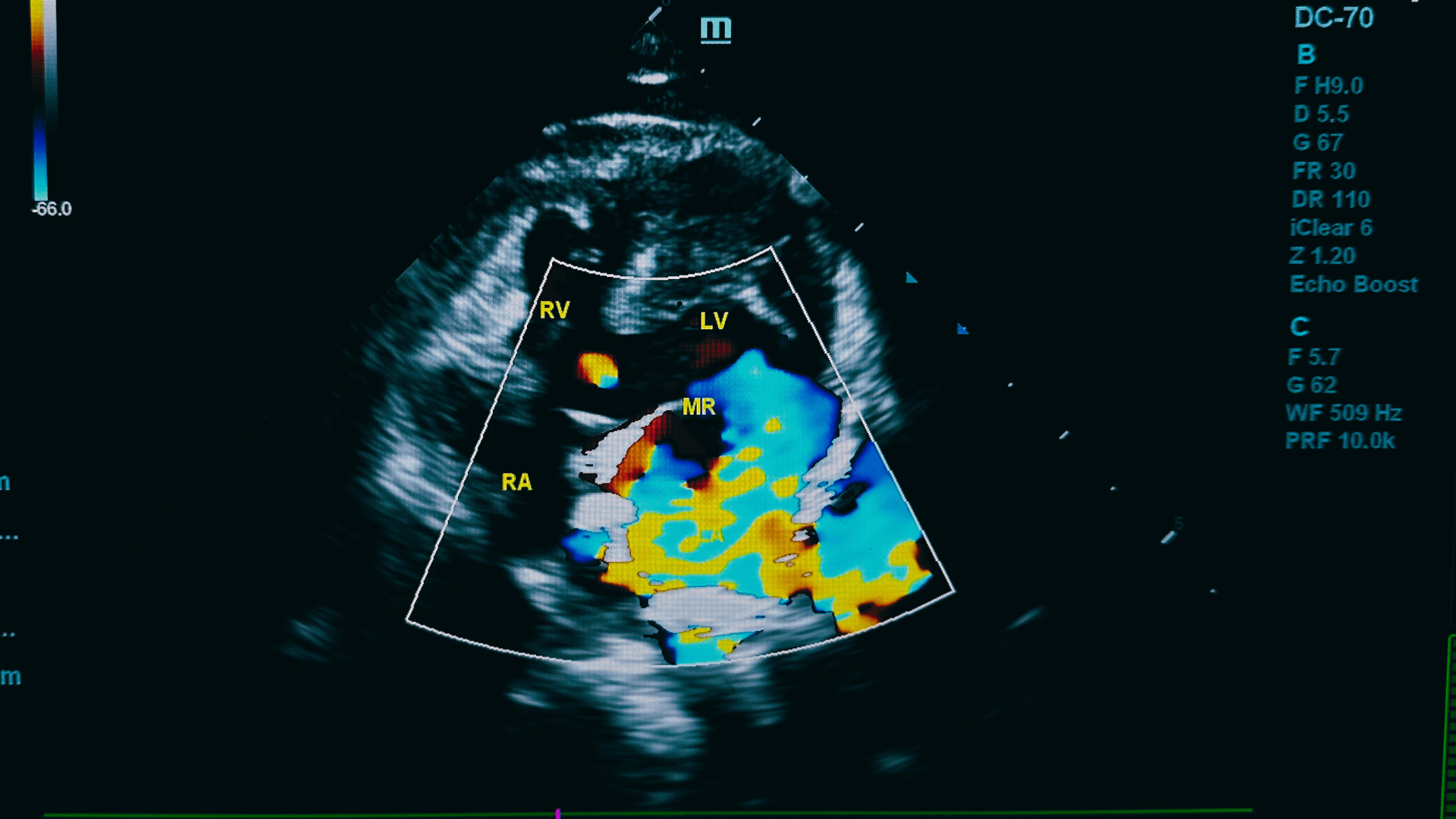
Cardiology Considerations with F12.20
Cannabis use can affect cardiovascular function, making cardiology CPT codes relevant in certain F12.20 cases. Healthcare providers may need to document cardiac evaluations when cannabis intoxication presents with cardiovascular symptoms.
| Cardiology CPT Code | Service Description | F12.20 Relevance |
| 93000 cpt code | Electrocardiogram, routine ECG with interpretation | Cardiac monitoring during intoxication |
| 93015 cpt code | Cardiovascular stress test | Exercise tolerance assessment |
| 93306 cpt code | Echocardiography, transthoracic | Cardiac function evaluation |
| 93224 cpt code | External electrocardiographic recording | Extended cardiac monitoring |
Medical professionals should consider cardiovascular effects when documenting F12.20 cases, particularly in patients with pre-existing heart conditions or those presenting with cardiac symptoms during cannabis intoxication.
Common Coding Errors with F12.20
Healthcare providers frequently make specific mistakes when applying F12.20 codes. These errors can result in claim denials or reduced reimbursement rates.
| Common Error | Impact | Prevention Strategy |
| Incorrect code selection | Claim denial | Verify intoxication presence |
| Insufficient documentation | Reduced reimbursement | Comprehensive clinical notes |
| Missing severity specification | Incomplete coding | Document disorder severity |
| Improper CPT code pairing | Billing errors | Verify service alignment |
| Timeline inconsistencies | Medical necessity questions | Clear temporal documentation |
Professional medical billing consultants can help identify and prevent these common F12.20 coding errors. MCB’s medical billing consulting services provide specialized expertise in substance use disorder billing.
Payer Requirements for F12.20 Claims
Different insurance companies maintain varying requirements for F12.20 claim processing. Healthcare providers must understand these requirements to achieve optimal reimbursement outcomes.
| Payer Type | Common Requirements | Processing Considerations |
| Medicare | Comprehensive documentation | Strict medical necessity standards |
| Medicaid | State-specific guidelines | Variable coverage policies |
| Commercial Insurance | Pre-authorization possible | Plan-specific limitations |
| Self-Pay | Direct billing | Payment plan considerations |
Healthcare providers should verify coverage benefits before treating patients with F12.20 diagnoses. Some insurance plans limit substance use disorder benefits or require specific treatment settings.
Quality Assurance for F12.20 Documentation
Proper F12.20 documentation requires systematic quality assurance processes. Healthcare organizations should implement review procedures to verify code accuracy and documentation completeness.
| Quality Measure | Review Criteria | Outcome Goal |
| Code Accuracy | Appropriate F12.20 assignment | Reduced claim denials |
| Documentation Quality | Complete clinical notes | Medical necessity support |
| CPT Code Alignment | Proper service coding | Optimal reimbursement |
| Compliance Standards | Regulatory adherence | Risk mitigation |
Regular auditing of F12.20 cases helps identify documentation gaps and coding inconsistencies. Healthcare providers can use these audits to improve their overall billing performance and reduce claim denials.
Technology Integration for F12.20 Billing
Modern Electronic Health Record (EHR) systems can streamline F12.20 documentation and billing processes. Healthcare providers should leverage technology to improve accuracy and efficiency.
| Technology Feature | F12.20 Application | Benefit |
| Clinical Decision Support | Code selection assistance | Improved accuracy |
| Documentation Templates | Standardized note formats | Comprehensive records |
| Billing Integration | Automated claim generation | Reduced errors |
| Analytics Reporting | Performance monitoring | Continuous improvement |
Healthcare organizations integrating F12.20 coding with advanced EHR systems typically achieve better reimbursement rates and fewer claim denials. Professional implementation services can help optimize these technological solutions.

Key Takeaways for F12.20 Code Management
Healthcare providers must master several critical aspects of F12.20 code application to achieve successful billing outcomes. Proper documentation serves as the foundation for accurate coding and optimal reimbursement.
The F12.20 code requires specific clinical documentation that supports both cannabis use disorder diagnosis and current intoxication symptoms. Healthcare providers should maintain comprehensive records that clearly demonstrate medical necessity for all services provided.
Professional medical billing services can significantly improve F12.20 claim outcomes through specialized expertise and systematic processes. These services help healthcare providers navigate complex payer requirements and maintain compliance standards.
Regular training and quality assurance processes help healthcare teams maintain proficiency in F12.20 coding and documentation requirements. Continuous education keeps providers current with changing regulations and best practices.
Technology integration can streamline F12.20 billing processes while improving accuracy and efficiency. Healthcare organizations should invest in systems that support comprehensive substance use disorder billing requirements.
MCB’s comprehensive suite of medical billing services includes specialized expertise in F12.20 coding and mental health billing. Our denial management services can help resolve complex F12.20 claim issues, while our medical credentialing services ensure providers maintain proper network participation for substance use disorder treatments. Contact MCB today to optimize your F12.20 billing processes and maximize your revenue cycle performance.