According to a landmark 2023 study in the Journal of Clinical Psychiatry, severe depression without psychotic features (F32.2) accounts for approximately 17% of all depression diagnoses but represents nearly 28% of denied claims in behavioral health practices.
This striking disparity highlights the critical importance of mastering F32.2 billing procedures. For mental health providers, this specific ICD-10 code is a financial linchpin that directly impacts practice sustainability and patient care.
Knowing exactly when and how to use F32.2 not only boosts reimbursement but also keeps you aligned with payer requirements. In short, applying this code correctly clearly conveys the seriousness of the patient’s condition and supports the care provided.
This comprehensive guide equips your practice with the precise knowledge needed to navigate F32.2 billing successfully transforming a potential reimbursement liability into a revenue opportunity while ensuring your severely depressed patients receive the intensive care they need.

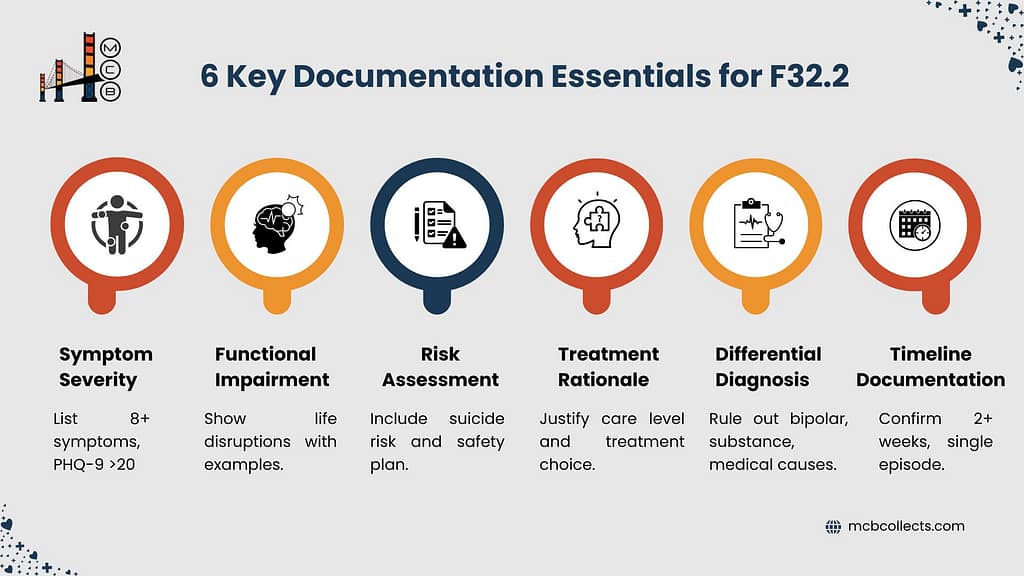
1. What is F32.2? Clinical Definition and Diagnostic Criteria
| Clinical Aspect | F32.2 Criteria |
| Official Designation | Major Depressive Disorder, single episode, severe without psychotic features |
| Diagnostic Category | Mood Disorders (F30-F39) |
| Episode Type | Single episode (as opposed to recurrent episodes coded elsewhere) |
| Severity Level | Severe |
| Key Distinction | Absence of psychotic features (unlike F32.3) |
| Diagnostic Requirements | • Depressed mood • Reduced energy • Decreased activity • Reduced capacity for enjoyment • Diminished concentration • Marked tiredness after minimal effort • Disturbed sleep • Diminished appetite • Lowered self-esteem • Self-guilt and/or worthlessness • Bleak and pessimistic view of the future |
| Minimum Symptoms | Patient must exhibit at least 8 of the symptoms listed above |
| Temporal Requirement | Symptoms present for at least 2 weeks |
| Functional Impact | Considerable difficulty continuing with ordinary activities |
Properly code F32.2 by demonstrating a severe depressive episode without psychosis, differentiating it from milder (F32.0, F32.1) and more severe (F32.3) presentations. Document substantial daily functioning impairment, excluding psychosis or significant psychomotor retardation. Look for pervasive emotional distress, significant loss of self-esteem and feelings of guilt, potential suicidal thoughts/attempts, and somatic symptoms as primary, not secondary, features of the depression.
The clinical presentation typically includes marked emotional distress with symptoms that dominate most aspects of life.
Patients may exhibit profound loss of self-esteem and feelings of uselessness or guilt. Suicidal thoughts and acts are common, alongside somatic symptoms. Unlike other depressive episodes coded with F41.1 (generalized anxiety disorder) or F43.10 (post-traumatic stress disorder), F32.2 represents depression that occurs as a primary condition rather than secondary to another disorder.
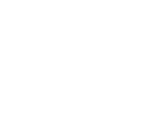
2. Billing Fundamentals for F32.2
| Billing Aspect | F32.2 Specifics |
| Billable Status | Confirmed billable/specific ICD-10-CM code |
| Implementation Date | October 1, 2015 (ICD-10) |
| Prior Coding Equivalent | 296.23 (ICD-9-CM) |
| Reimbursement Category | Generally well-recognized by most payers |
| Documentation Requirements | • Clear establishment of severity criteria • Evidence of functional impairment • Absence of psychotic features • Treatment plan appropriate to severity |
| Claim Form Placement | Box 21 (diagnosis) on CMS-1500 claim form |
| Supporting Service Codes | Frequently billed with psychotherapy CPT codes (90832, 90834, 90837) |
| Medical Necessity Requirements | Higher levels of service typically justified with F32.2 vs. milder codes |
| Frequency Limitations | Generally not subject to frequency edits by payers |
| Common Denial Reasons | • Insufficient documentation of severity • Missing elements of diagnostic criteria • Contradictory clinical information |
F32.2 is a fully billable diagnosis code approved for medical reimbursement purposes. Unlike some other psychiatric codes that may trigger payer scrutiny, F32.2 is widely accepted when properly documented. The key to successful billing lies in establishing the severity of the depression without introducing elements that would suggest psychotic features better captured by F32.3 or comorbid conditions like F10.20 (alcohol dependence) that might complicate the clinical picture.
When billing F32.2 with psychotherapy services, practices should select appropriate CPT codes that match the service intensity to the diagnosis severity. For example, longer psychotherapy sessions (90837) are often more readily justified with severe diagnoses like F32.2 compared to milder presentations. For initial evaluations, comprehensive psychiatric diagnostic procedures (90791 or 90792) provide the assessment depth necessary to establish this diagnosis.
Practice management systems should be configured to link F32.2 with appropriate service intensity levels and documentation templates that prompt clinicians to record all elements necessary for diagnostic justification.
This systematic approach helps avoid the common pitfall of selecting a severe diagnosis code without including the corresponding documentation to support it a frequent trigger for denial of services that could otherwise be properly reimbursed.
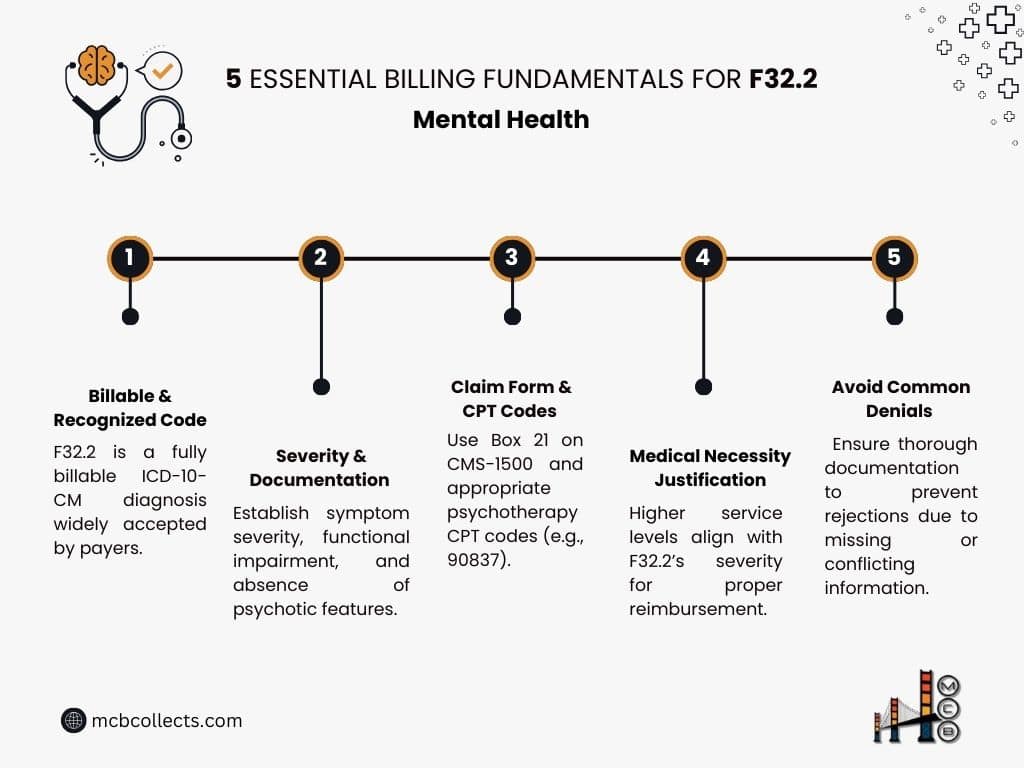
3. F32.2 in Practice: Clinical Documentation Requirements
| Documentation Element | Required Components for F32.2 |
| Symptom Severity | • Detailed description of at least 8 severe depressive symptoms • Explicit statement regarding absence of psychotic features • Quantification of symptom impact using standardized measures (e.g., PHQ-9 scores >20) |
| Functional Impairment | • Specific examples of impairment across multiple life domains • Documentation of considerable difficulty with ordinary activities • Comparative assessment to patient’s baseline functioning |
| Risk Assessment | • Comprehensive suicide risk evaluation • Documentation of safety planning if suicidal ideation present • Assessment of self-care capacity |
| Treatment Rationale | • Justification for level of care selected • Explanation of why less intensive interventions insufficient • Clear connection between F32.2 diagnosis and treatment plan |
| Differential Diagnosis | • Documentation ruling out bipolar disorder (F31.9) • Assessment for substance-induced mood disorder • Consideration of medical causes of depression |
| Timeline Documentation | • Onset and duration of current depressive episode • Confirmation episode exceeds minimum 2-week requirement • Documentation that this is a single (not recurrent) episode |
The F32.2 diagnosis calls for detailed documentation that clearly establishes the severe nature of the depressive episode while explicitly noting the absence of psychotic features.
Auditors reviewing claims with an F32.2 diagnosis require comprehensive assessment notes detailing quantified symptom severity and functional impairment.
Unlike F32.1, F32.2 necessitates demonstrating substantial impact across multiple life domains. Documentation must include validated assessment measures, such as PHQ-9 scores above 20, or GAF scores in the 40-50 range, to objectively support the severe classification.
Common documentation pitfalls when using F32.2 include:
- Inconsistent severity indicators: Notes describing a patient as “mildly distressed” or “maintaining daily functions adequately” contradict the F32.2 severity level and trigger immediate denials.
- Missing functional impairment details: Vague statements about impairment without specific examples fail to support the F32.2 diagnosis. Documentation should include concrete examples such as “patient has missed 12 days of work in the past month due to depressive symptoms” rather than generalized statements.
- Contradictory clinical information: Documentation mentioning psychotic features (hallucinations, delusions) while using F32.2 creates a coding contradiction, as such symptoms would warrant F32.3 instead.
- Insufficient symptom count: F32.2 requires documentation of a sufficient number of symptoms (typically at least 8 from the diagnostic criteria) to establish the severe classification.
- Overlooking temporal requirements: Failing to document that symptoms have persisted for at least two weeks undermines the diagnostic validity.
Best practices for supporting medical necessity with F32.2 include creating a clear narrative that links symptom severity to the selected interventions. This narrative should explain why the particular treatment approach is necessary given the severe nature of the depression. For example, when billing more intensive services like 90837 (60-minute psychotherapy), documentation should explain why shorter sessions would be insufficient given the complexity and severity of the patient’s F32.2 presentation.
4. Coding Relationships: F32.2 and Associated Codes
| Relationship Type | Associated Codes with F32.2 |
| Hierarchical Relationship | • F32 (Parent category: Depressive episode) • F30-F39 (Mood [affective] disorders category) |
| Severity Variants | • F32.0 (Mild depressive episode) • F32.1 (Moderate depressive episode) • F32.3 (Severe depressive episode with psychotic symptoms) |
| Common Comorbidities | • F41.1 (Generalized anxiety disorder) • F42 (Obsessive-compulsive disorder) • F43.10 (Post-traumatic stress disorder) • F10.20 (Alcohol dependence) • F11.20 (Opioid dependence) |
| Potential Progression Codes | • F33.2 (Recurrent depressive disorder, current episode severe without psychotic symptoms) • F33.3 (Recurrent depressive disorder, current episode severe with psychotic symptoms) |
| Exclusion Codes | • F31.9 (Bipolar affective disorder, unspecified) • F06.3 (Organic mood disorder) • F99 (Mental disorder, not otherwise specified) |
Understanding F32.2’s relationship to other diagnostic codes is essential for accurate billing and clinical documentation. F32.2 belongs to the F32 subset of codes, which specifically identify depressive episodes that occur as single (rather than recurrent) episodes. This distinction is crucial, as patients with a history of previous depressive episodes should be coded within the F33 series instead.
The severity spectrum within the F32 family moves from F32.0 (mild) through F32.1 (moderate) to F32.2 (severe without psychotic features) and finally F32.3 (severe with psychotic features).
When selecting between these codes, clinicians must carefully assess symptom count, functional impact, and the presence or absence of psychotic features. The differences in reimbursement and treatment expectations across this spectrum can be significant, with F32.2 typically justifying more intensive interventions than F32.0 or F32.1.
Unlike F32.3, which includes hallucinations, delusions, or depressive stupor, F32.2 represents severe depression where reality testing remains intact. This distinction has important implications for treatment planning and billing justification. Services like psychological testing are often more readily approved for complex diagnostic scenarios where distinguishing between F32.2 and F32.3 is clinically significant.
F32.2 frequently co-occurs with anxiety disorders (F41.1), substance use disorders (F10.20-F12.20), and trauma-related conditions (F43.10). When documenting multiple diagnoses, establishing a clear primary diagnosis is essential for proper billing sequence. If F32.2 is the primary focus of treatment, it should be listed first on claims, followed by secondary conditions that may complicate treatment.
For pediatric populations, careful consideration should be given to developmental presentations of depression versus neurodevelopmental disorders like F84.0 (Autism spectrum disorder) or F90.0 (Attention-deficit hyperactivity disorder), which can present with mood symptoms but require different treatment approaches and may have different reimbursement profiles.
5. F32.2 Billing Challenges and Solutions
| Billing Challenge | Strategic Solutions for F32.2 |
| Insufficient Severity Documentation | • Implement structured assessment tools (PHQ-9, HAM-D) • Create F32.2-specific documentation templates • Develop severity scoring systems aligned with ICD-10 criteria |
| Medical Necessity Denials | • Link treatment intensity to documented severity • Provide explicit rationale for chosen interventions • Include functional impairment impact statements |
| Service Intensity Mismatches | • Align CPT code selection with F32.2 severity • Document why lower-level services insufficient • Create crosswalk guides for clinicians |
| Payer-Specific Limitations | • Maintain payer-specific F32.2 policy database • Pre-authorize services when required • Develop payer-specific documentation templates |
| Recurrent vs. Single Episode Confusion | • Implement comprehensive intake history protocols • Document clear timeline of previous episodes • Create decision support tools for F32 vs. F33 selection |
Billing for services associated with F32.2 presents unique challenges that require strategic approaches to ensure clean claims and appropriate reimbursement. One of the most common rejection reasons for F32.2 claims is insufficient documentation of severity criteria. Payers increasingly require explicit documentation that matches the precise language of the ICD-10 diagnostic criteria, particularly when the diagnosis supports higher-level service codes like 90837 or 90839 for crisis intervention.
To address documentation challenges, practices should implement structured assessment protocols that generate quantifiable measures of depression severity. This might include routine use of the Hamilton Depression Rating Scale (HAM-D) or Montgomery–Åsberg Depression Rating Scale (MADRS), with score thresholds clearly documented to support the F32.2 severity classification. These standardized measures provide objective support for the clinical judgment and strengthen claims justification.
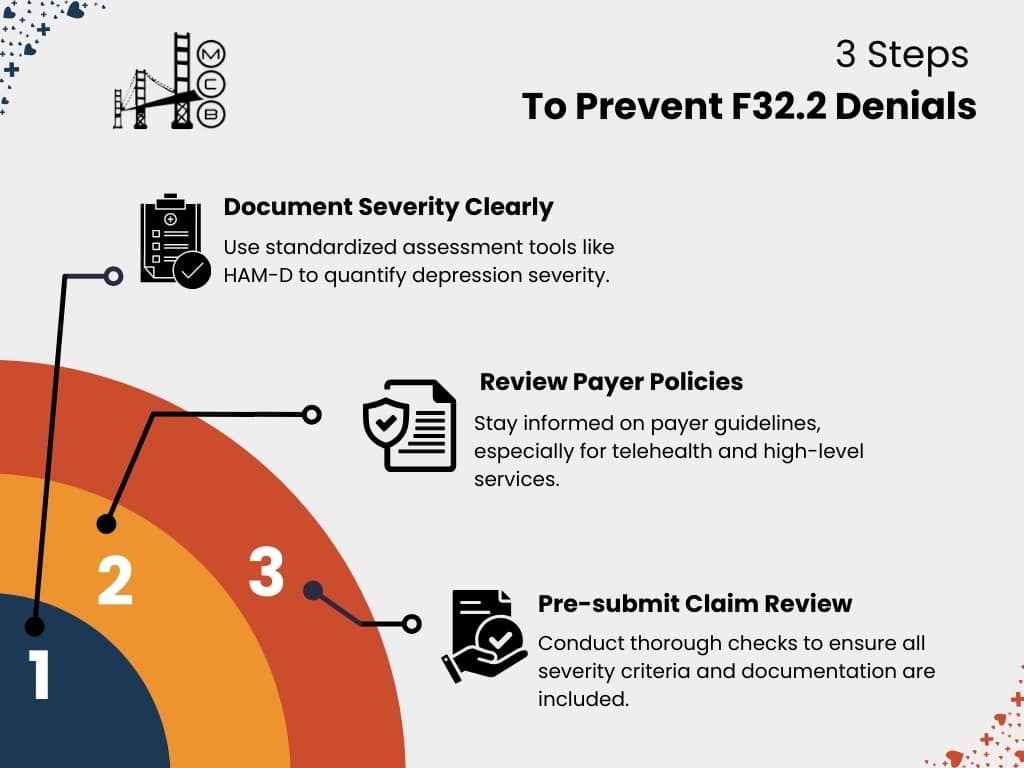
Another common challenge occurs when billing F32.2 with telehealth services. While telehealth has expanded dramatically, some payers maintain restrictions on telehealth for severe mental health conditions, creating potential denials when F32.2 is billed with virtual check-in codes like G2012 or G2010.
Practices should maintain updated payer policies regarding telehealth limitations for severe depression and ensure proper place of service coding for telehealth F32.2 claims.
When facing denials for F32.2 claims, a structured appeals process should include:
- Clinical documentation enhancement: Supplement appeals with additional severity documentation, including standardized assessment scores and functional impact statements.
- Coding validation: Provide ICD-10 guidelines that support the F32.2 selection based on documented symptoms and severity.
- Literature support: Include references to clinical practice guidelines that recommend specific treatments for severe depression to support medical necessity.
- Peer-to-peer reviews: For high-value denied claims, request peer-to-peer reviews where treating clinicians can directly explain the clinical decision-making that supports both the F32.2 diagnosis and associated services.
To prevent denials, behavioral health practices should implement pre-submission claim reviews specifically for F32.2 services, creating a checklist that ensures all severity criteria and supporting documentation are present before claim submission. This proactive approach reduces denial rates and accelerates reimbursement for these clinically complex services.
6. Maximizing Reimbursement for F32.2 Services
| Reimbursement Strategy | Implementation for F32.2 |
| Payer Contract Analysis | • Review fee schedules for F32.2-associated services • Negotiate carve-outs for severe depression treatment • Identify payers with depression care incentive programs |
| Comprehensive Documentation | • Develop severity-specific templates • Include quantitative assessment measures • Document medical necessity for each service level |
| Service Diversification | • Expand billable services for severe depression • Consider group therapy (90853) as adjunctive treatment • Implement family therapy (90847) when appropriate |
| Outcome Tracking | • Document symptom improvement over time • Link interventions to specific outcome measures • Demonstrate value-based care metrics |
| Denial Pattern Analysis | • Track F32.2-specific denial reasons • Identify provider-specific documentation patterns • Implement targeted training for problem areas |
Maximizing reimbursement for F32.2 services requires a sophisticated approach that recognizes the varying requirements and opportunities across different payer types. Commercial payers, Medicare, and Medicaid may each have specific documentation expectations for F32.2, necessitating a payer-specific strategy for optimal reimbursement.
For Medicare beneficiaries, F32.2 often qualifies patients for more intensive services under the Psychiatric Collaborative Care Model (CoCM), which provides additional reimbursement opportunities beyond traditional psychotherapy.
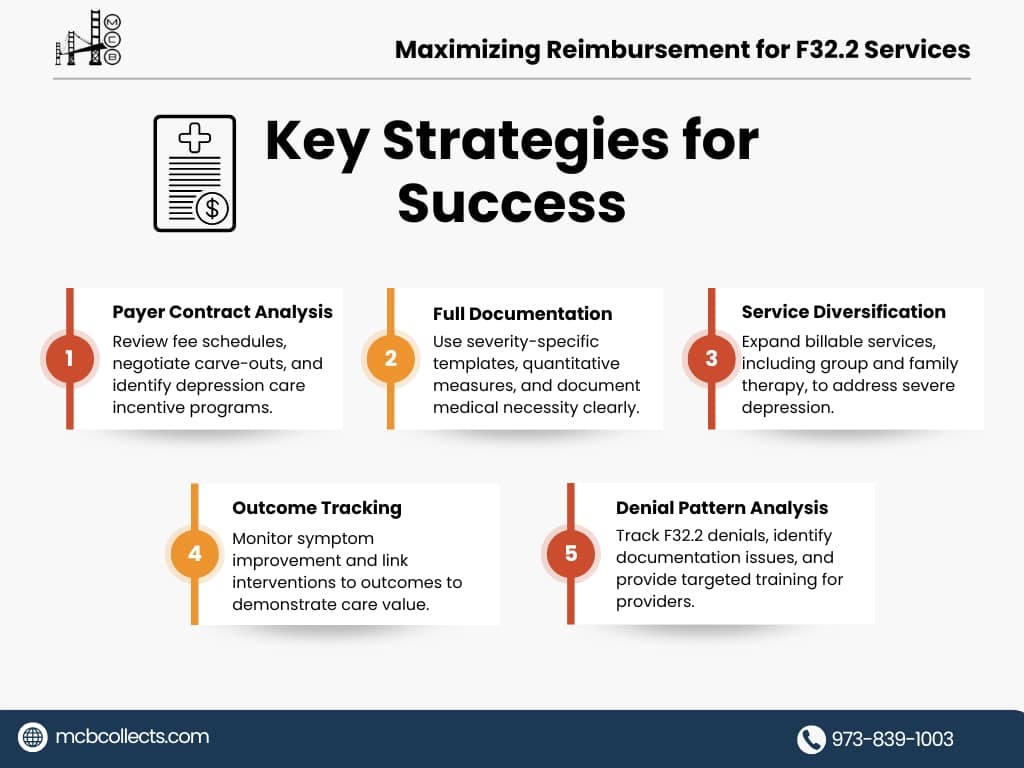
Practices should evaluate whether their severely depressed Medicare patients qualify for these programs and document accordingly to support these higher-reimbursing service codes.
Commercial payers increasingly implement specific medical policies for severe depression treatment that may include step therapy requirements or prior authorization protocols.
Practice management systems should be configured to flag F32.2 diagnoses for pre-submission review, ensuring all payer-specific requirements are met before claims submission. This proactive approach significantly improves first-pass payment rates for F32.2-related services.
Documentation strategies that support optimal payment include:
- Severity progression tracking: Document changes in symptom severity over time, particularly when patients improve from F32.2 to less severe classifications. This demonstrates treatment effectiveness and justifies the services provided.
- Treatment resistance documentation: For patients who maintain an F32.2 diagnosis despite treatment, clearly document treatment resistance factors that necessitate continued intensive intervention.
- Functional impact specificity: Rather than general statements about impairment, document specific functional limitations in occupational, social, and self-care domains that correlate with the F32.2 severity level.
- Risk factor documentation: Clearly document factors that contribute to severity or complicate treatment, such as chronic pain, social determinants of health, or limited support systems.
For practices using family therapy or multiple provider types in treating F32.2, clear documentation of each provider’s distinct contribution to addressing the severe depression is essential. This becomes particularly important when billing for both individual therapy and group therapy or when psychiatric services and psychological testing services are provided concurrently.
Monitoring reimbursement patterns for F32.2 services should be a routine part of practice management. Regular analysis of payment rates, denial reasons, and adjudication timeframes specific to F32.2 claims allows practices to identify and address problematic patterns before they significantly impact revenue.
Conclusion: Optimizing F32.2 Billing for Practice Success
The F32.2 diagnosis code represents a critical tool for behavioral health providers treating patients with severe depression. When properly documented and billed, F32.2 facilitates appropriate reimbursement for the intensive services these complex patients require. However, the code’s specificity demands careful attention to diagnostic criteria, documentation standards, and payer requirements.
By implementing structured documentation protocols, comprehensive staff training, and strategic billing practices specific to F32.2, practices can significantly improve both compliance and revenue cycle performance. The distinction between F32.2 and other depression codes carries meaningful clinical and financial implications that directly impact practice sustainability.

If your practice struggles with F32.2 denials, delayed payments, or documentation challenges, MCB’s team of behavioral health billing specialists can implement customized solutions tailored to your specific clinical population and payer mix.
Our comprehensive process design and accountability mechanisms ensure that every F32.2 claim is optimally documented, properly coded, and strategically submitted for maximum reimbursement.
Contact MCB today to discover how our specialized behavioral health billing services can help your practice transform F32.2 challenges into reimbursement opportunities, allowing you to focus on providing the high-quality care your severely depressed patients need while we ensure you receive appropriate compensation for these complex services.