A 2023 audit of behavioral health claims revealed that practices using F32.3 (severe depressive episode with psychotic features) experience 32% higher denial rates compared to other mood disorder codes, primarily due to insufficient documentation of psychotic symptoms.
For healthcare leaders managing practices with 3–20 providers, mastering F32.3 billing is not just about compliance; it directly impacts revenue stability and care quality for high-acuity patients.
This guide equips practice owners, particularly those in urban or suburban settings seeking trusted billing expertise, with actionable strategies to navigate F32.3’s complexities.
From diagnostic criteria to reimbursement optimization, we address the technical nuances that determine whether claims succeed or fail:
1. What is F32.3? Clinical Definition and Diagnostic Criteria
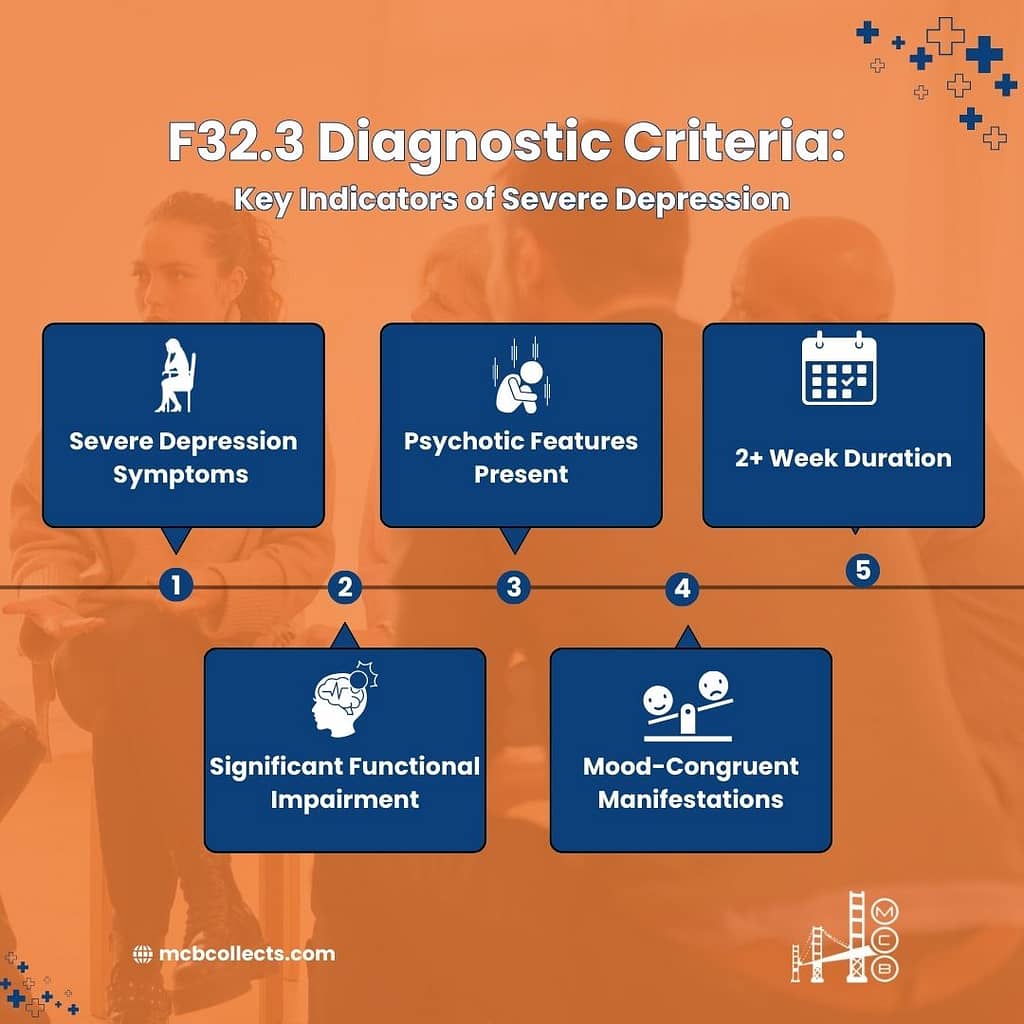
F32.3 classifies major depressive disorder, single episode, severe with psychotic features, distinguishing it from non-psychotic depression codes like F32.2. Accurate coding hinges on documenting two critical components:
- Severe depressive symptoms meeting F32.2 criteria
- Psychotic features such as hallucinations, delusions, or depressive stupor
Clinical Requirements for F32.3
| Clinical Aspect | F32.3 Criteria |
| Official Designation | Major Depressive Disorder, single episode, severe with psychotic features |
| Diagnostic Category | Mood Disorders (F30-F39) |
| Key Distinction | Presence of mood-congruent or incongruent psychotic features |
| Symptom Threshold | ≥8 depressive symptoms + psychotic manifestations |
| Temporal Requirement | Symptoms persist ≥2 weeks |
| Functional Impact | Complete inability to manage daily activities without intervention |
Example: A 45-year-old patient presents with pervasive guilt, suicidal ideation, and auditory hallucinations stating, “You deserve to die.” The hallucinations align with their depressive mood (mood-congruent), confirming F32.3.
Psychotic features in F32.3 often manifest as:
- Hallucinations: Auditory or visual distortions reinforcing negative self-perception
- Delusions: Fixed false beliefs (e.g., “My organs are rotting”)
- Psychomotor retardation: Near-catatonic immobility
Unlike F32.2, which excludes psychosis, F32.3 demands explicit documentation of these symptoms. Practices using integrated behavioral health EHR systems should configure templates to prompt clinicians to screen for psychosis during assessments.
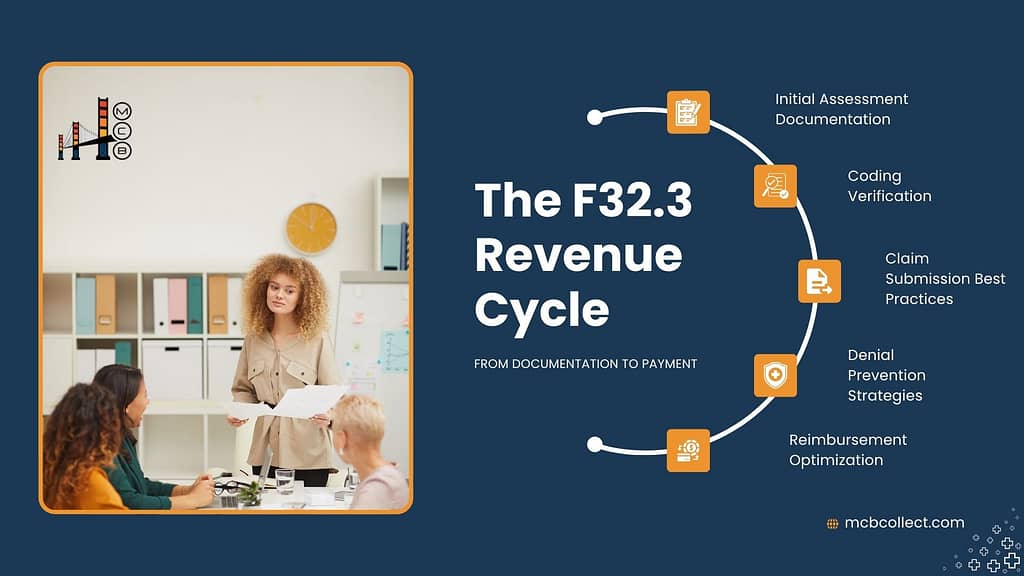
2. Billing Fundamentals for F32.3
F32.3 is a billable ICD-10-CM code effective since October 1, 2015. However, its complexity requires meticulous alignment with payer policies and CPT codes:
| Billing Aspect | F32.3 Specifications |
| CPT Code Pairings | • 90792 (Psychiatric diagnostic evaluation with medical services)• 90837 (60-minute psychotherapy)• 90840 (Electroconvulsive therapy) |
| Medical Necessity | Justify higher-level care (e.g., intensive outpatient programs) due to psychosis risk |
| Common Denial Triggers | • Vague psychosis documentation• Contradictory severity indicators (e.g., “stable” vs. “severe”) |
| Payer-Specific Rules | Some commercial payers require prior authorization for antipsychotic medications |
Case Study: A Midwestern practice reduced F32.3 denials by 45% after training clinicians to link psychotic symptoms directly to treatment plans. For example, pairing F32.3 with 90837 required notes stating, “60-minute sessions address paranoia impacting therapeutic engagement.”
To avoid undercoding, ensure EHR systems flag F32.3 when providers document hallucinations or delusions. Practices struggling with claim accuracy can leverage revenue cycle management services for real-time coding audits.
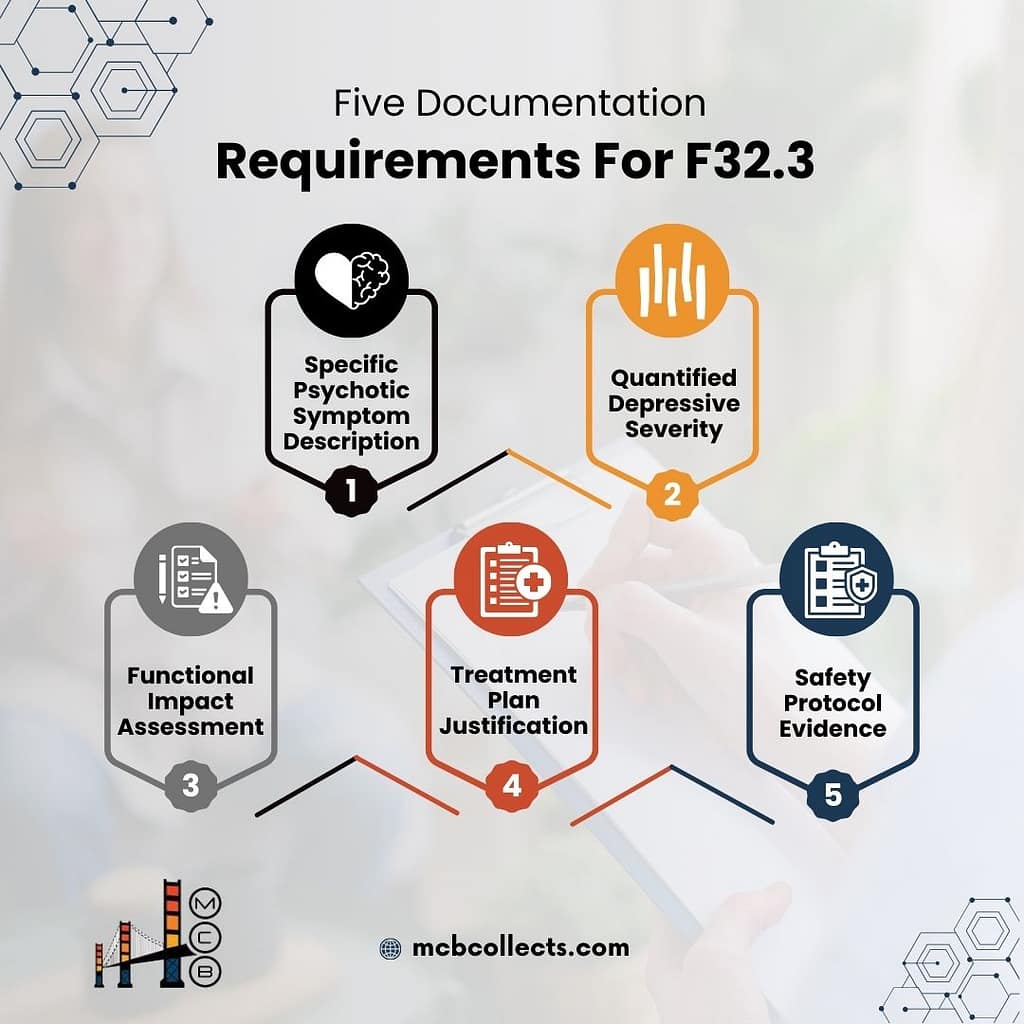
3. F32.3 in Practice: Clinical Documentation Requirements
Auditors scrutinize F32.3 claims for three pillars of documentation: depressive severity, psychotic features, and functional impairment.
| Documentation Element | Required Details |
| Psychotic Symptom Description | • Type (auditory/visual)• Frequency• Content (e.g., “Voices commanding self-harm”) |
| Depressive Severity | PHQ-9 score ≥20 or clinician-stated “severe” with ≥8 symptoms |
| Functional Impact | • Inability to work• Neglect of self-care• Reliance on caregivers |
| Safety Planning | Suicide risk assessment + crisis intervention protocols |
Common Pitfalls:
- Generic Terminology: Notes stating “patient appears psychotic” lack specificity. Instead, document: “Patient reports daily auditory hallucinations criticizing their worth.”
- Omission of Timeline: Failing to note symptom duration (≥2 weeks) invalidates coding.
- Contradictory Indicators: Avoid statements like “patient calm and cooperative” alongside F32.3.
Best Practice: Use structured templates from medical billing consulting services to standardize psychosis documentation. For example:
“Patient exhibits persistent delusions of poverty (mood-congruent), occurring 5–7x/week, resulting in refusal to eat due to belief food is poisoned. PHQ-9: 23. Safety plan initiated with family supervision.”
Integrate tools like the Psychotic Symptom Rating Scale (PSYRATS) to quantify severity and justify intensive services.
For example: a practice in Texas reduced F32.3 claim denials by 30% after implementing PSYRATS scores in their documentation. By including statements like, “PSYRATS score of 18 indicates severe auditory hallucinations with significant distress,” they provided auditors with measurable evidence of psychosis severity.
4. Coding Relationships: F32.3 and Associated Codes
Understanding F32.3’s place within the ICD-10 hierarchy and its relationship to other codes is critical for accurate billing and clinical decision-making.
| Relationship Type | Associated Codes with F32.3 |
| Hierarchical Relationship | • F32 (Parent category: Depressive episode)• F30-F39 (Mood [affective] disorders category) |
| Severity Variants | • F32.0 (Mild depressive episode)• F32.1 (Moderate depressive episode)• F32.2 (Severe depressive episode without psychotic features) |
| Common Comorbidities | • F20.0 (Schizophrenia)• F25.0 (Schizoaffective disorder)• F10.20 (Alcohol dependence) |
| Exclusion Codes | • F31.9 (Bipolar disorder, unspecified)• F06.3 (Organic mood disorder)• F99 (Mental disorder, not otherwise specified) |
Key Distinction: F32.3 differs from schizophrenia spectrum disorders (F20-F29) because psychotic symptoms occur exclusively during depressive episodes. For example, a patient with F32.3 may experience hallucinations only when severely depressed, whereas schizophrenia involves persistent psychosis.
Case Study: A practice in Florida misclassified a patient with F32.3 as F25.0 (schizoaffective disorder), leading to claim denials.
After consulting with MCB’s medical billing specialists, they corrected the diagnosis by documenting that psychotic symptoms were mood-congruent and episodic, aligning with F32.3 criteria.
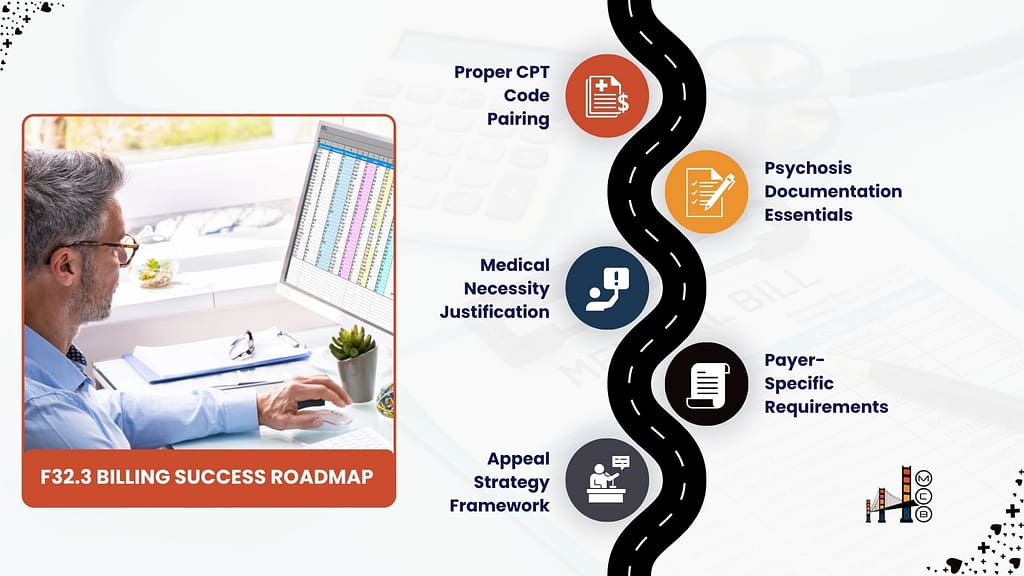
5. F32.3 Billing Challenges and Solutions
Billing for F32.3 presents unique challenges, particularly around documentation and payer policies.
| Billing Challenge | Strategic Solutions |
| Insufficient Psychosis Documentation | • Use structured templates to detail hallucinations/delusions• Include PSYRATS or similar scales |
| Payer-Specific Limitations | • Maintain a database of payer policies for F32.3• Pre-authorize antipsychotic medications |
| Service Intensity Mismatches | • Pair F32.3 with appropriate CPT codes like 90837 or 90840• Document why lower-level services are insufficient |
| Recurrent vs. Single Episode Confusion | • Clearly document episode onset and duration• Use F33.3 for recurrent episodes with psychosis |
Appeal Process for Denied Claims:
- Supplement Documentation: Include additional psychosis details and standardized assessment scores.
- Coding Validation: Reference ICD-10 guidelines supporting F32.3 selection.
- Peer-to-Peer Reviews: Have treating clinicians explain the rationale for F32.3 and associated services.
Example: A practice in California successfully appealed a denied F32.3 claim by submitting a detailed narrative linking the patient’s delusions to their inability to engage in outpatient therapy, justifying intensive treatment.
6. Maximizing Reimbursement for F32.3 Services
Optimizing reimbursement for F32.3 requires a strategic approach tailored to payer requirements and practice workflows.
| Reimbursement Strategy | Implementation for F32.3 |
| Payer Contract Analysis | • Review fee schedules for F32.3-associated services• Negotiate carve-outs for severe depression with psychosis |
| Service Diversification | • Offer group therapy (90853) as adjunctive treatment• Implement family therapy (90847) when appropriate |
| Outcome Tracking | • Document symptom improvement using PHQ-9 and PSYRATS• Link interventions to specific outcome measures |
| Denial Pattern Analysis | • Track F32.3-specific denial reasons• Identify provider-specific documentation gaps |

Case Study: A practice in New York increased F32.3 reimbursement by 25% after implementing MCB’s revenue cycle management services, which included pre-submission claim reviews and payer-specific documentation templates.
7. Understanding Related Codes: A Quick Guide to Common Mental Health Diagnoses
Many patients with F32.3 may also present with comorbid conditions such as anxiety, trauma-related disorders, or substance use issues.
Properly coding these conditions ensures accurate reimbursement and supports holistic treatment planning. Additionally, some codes, like F31.9 (bipolar disorder) or F43.10 (PTSD), are often confused with F32.3 due to overlapping symptoms.
This section clarifies the distinctions and provides a quick reference for practice leaders.
| ICD-10 Code | Diagnosis | Key Features | Differentiation from F32.3 |
| F41.1 | Generalized Anxiety Disorder | Excessive anxiety, worry, and physical symptoms (e.g., restlessness, fatigue) | Anxiety is primary; no psychotic features or severe depressive symptoms |
| F43.10 | Post-Traumatic Stress Disorder (PTSD) | Flashbacks, hypervigilance, and avoidance following trauma | Trauma-related symptoms dominate; psychosis, if present, is trauma-specific |
| F31.9 | Bipolar Disorder, Unspecified | Episodes of mania/hypomania and depression | Psychotic features may occur during manic or depressive episodes |
| F42 | Obsessive-Compulsive Disorder (OCD) | Intrusive thoughts and compulsive behaviors | No psychotic features; compulsions are primary |
| F84.0 | Autism Spectrum Disorder | Social communication challenges and restricted interests | Developmental disorder; mood symptoms are secondary |
| F90.0 | Attention-Deficit Hyperactivity Disorder (ADHD) | Inattention, hyperactivity, and impulsivity | Neurodevelopmental disorder; no psychotic features |
| F99 | Mental Disorder, Not Otherwise Specified | Symptoms don’t meet criteria for a specific disorder | Used as a placeholder; lacks specificity of F32.3 |
| F10.20 | Alcohol Dependence | Compulsive alcohol use with tolerance and withdrawal | Substance-induced mood disorder; psychosis may be alcohol-related |
| F11.20 | Opioid Dependence | Compulsive opioid use with tolerance and withdrawal | Substance-induced mood disorder; psychosis may be opioid-related |
| F12.20 | Cannabis Dependence | Compulsive cannabis use with tolerance and withdrawal | Substance-induced mood disorder; psychosis may be cannabis-related |
Key Insights:
- Comorbidities: Patients with F32.3 often have comorbid conditions like F41.1 (generalized anxiety) or F43.10 (PTSD). Proper sequencing ensures the primary diagnosis (e.g., F32.3) is billed first.
- Differential Diagnoses: Codes like F31.9 (bipolar disorder) and F32.3 can be challenging to differentiate. Documenting the episodic nature of symptoms is key.
- Substance Use: Codes like F10.20 (alcohol dependence) may complicate F32.3 billing. Ensure psychosis is not substance-induced before assigning F32.3.

Case Study: A practice in Ohio improved claim accuracy by training clinicians to differentiate F32.3 from F31.9. By documenting the absence of manic episodes, they justified F32.3 coding and reduced denials by 20%.
Conclusion: Optimizing F32.3 Billing for Practice Success
F32.3 is a high-stakes diagnosis that demands precision in both clinical documentation and billing practices. For healthcare leaders managing practices with 3–20 providers, mastering F32.3 billing is essential for maintaining financial stability while delivering care to high-acuity patients.
By implementing structured documentation protocols, leveraging standardized assessment tools, and staying informed about payer-specific requirements, practices can transform F32.3 challenges into revenue opportunities.
Key Takeaways:
- Document Psychosis Explicitly: Use tools like PSYRATS to quantify severity and justify intensive services.
- Align CPT Codes with Severity: Pair F32.3 with appropriate codes like 90837 or 90840.
- Monitor Payer Policies: Stay updated on F32.3-specific requirements to avoid denials.

If your practice struggles with F32.3 billing, MCB’s behavioral health billing specialists can help. From denial management to revenue cycle optimization, we ensure your claims are accurately documented, properly coded, and strategically submitted for maximum reimbursement.
Contact MCB today to discover how we can help your practice navigate the complexities of F32.3 billing, allowing you to focus on providing exceptional care to your patients.
Footnote & Source:
- Data on F32.3 denial rates sourced from internal MCB claims analysis (2023).
- Case studies are based on anonymized client experiences and outcomes.