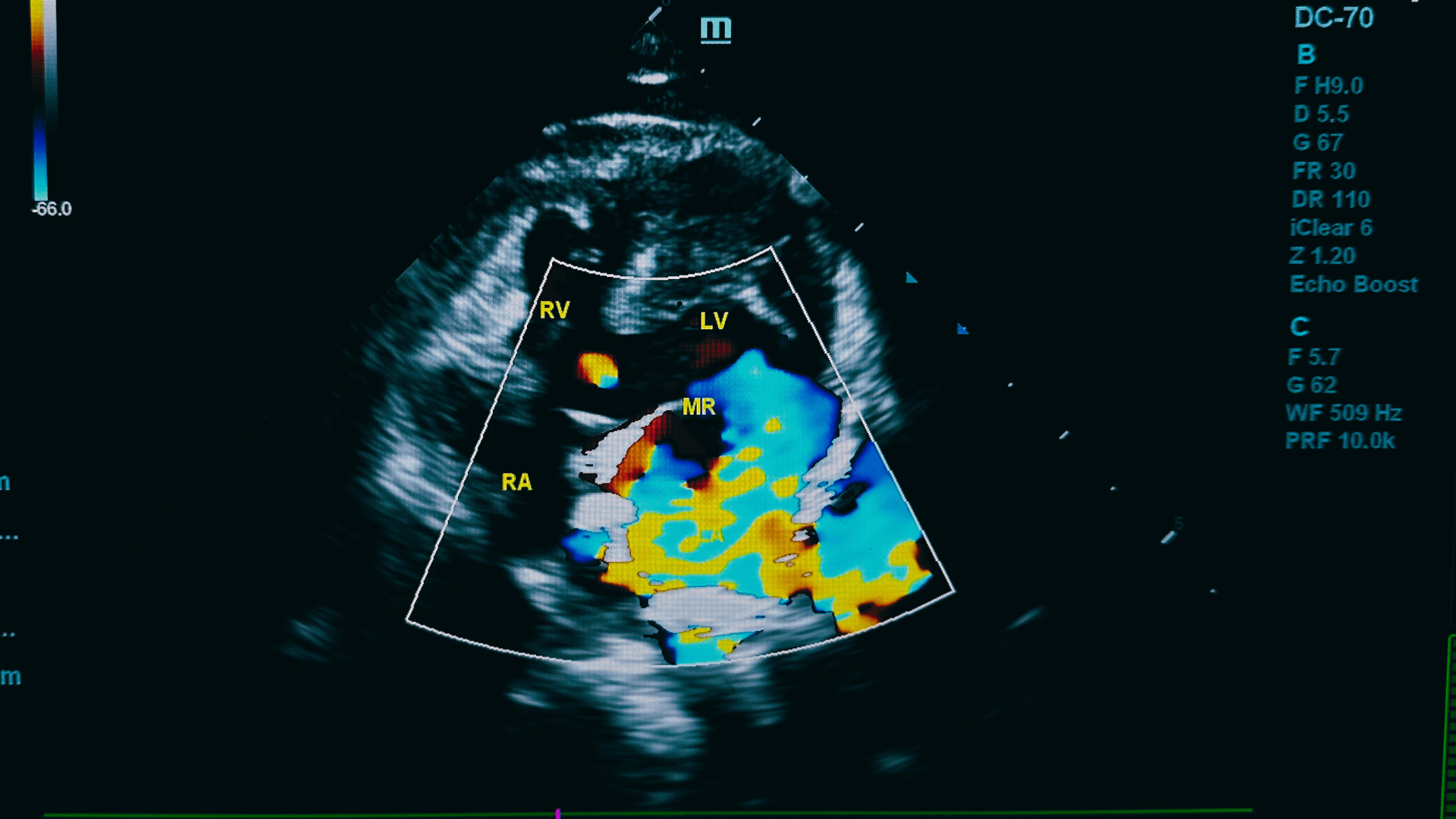
93016 CPT Code represents a critical component of cardiac stress testing procedures. This code covers the oversight and interpretation portion of stress tests.
Healthcare providers use this code when they oversee patient monitoring during exercise or pharmacological stress testing.
The code applies treadmill and bicycle stress tests. Proper documentation and billing practices help you avoid claim denials and payment delays.
What is the 93016 CPT Code?
93016 CPT Code is used when a doctor watches over a heart stress test and reads the results. It means the doctor is present during the test to make sure everything goes safely and then explains what the test shows.
If you need help with other cardiac-related billing codes, you can check out our article about the 93015 CPT code for complete stress test procedures.
CPT Code 93016 Basic Information
Code Element | Details |
CPT Code | 93016 |
Category | Medicine – Cardiovascular |
Code Type | Professional Service |
Billable Status | Active |
Medicare Coverage | Yes (with proper documentation) |
Typical Setting | Outpatient, Hospital |
When to Use 93016 CPT Code?
Healthcare providers use CPT 93016 in specific clinical situations. The code applies when a physician provides direct supervision during stress testing.
The physician must be present during the entire procedure. They monitor the patient’s vital signs and watch for any adverse reactions.
Appropriate Use Cases | Documentation Required |
Treadmill stress test supervision | Patient monitoring notes |
Bicycle exercise test oversight | Vital sign documentation |
Pharmacological stress supervision | Adverse reaction monitoring |
Nuclear stress test monitoring | Safety protocol compliance |
Documentation Requirements for CPT 93016
Proper documentation protects against claim denials. Insurance companies review medical records to verify the service provided.
The physician must document their direct involvement in the procedure. Records should show continuous patient monitoring throughout the test.
Required Documentation | Specific Elements |
Physician presence | Time in and time out |
Patient monitoring | Vital signs every stage |
Safety protocols | Emergency procedures ready |
Clinical decision-making | Test continuation decisions |
For guidance on proper medical documentation practices, you can check out our article about F99 diagnosis code documentation requirements.
Billing Guidelines for 93016 CPT Code
CPT 93016 follows specific billing rules. These guidelines help avoid common billing errors and claim denials.
The code cannot be billed with certain other procedures. Understanding these restrictions prevents payment issues.
Billing Rule | Application |
One unit per test | Never bill multiple units |
Professional component only | Technical component separate |
Supervision required | Physician must be present |
Same-day restrictions | Check bundling rules |
Common Billing Errors with 93016 CPT Code
Medical billing staff often make mistakes with this code. These errors lead to claim denials and delayed payments.
The most common error involves billing without proper supervision documentation. Insurance companies frequently deny these claims.
Common Error | Solution |
Missing supervision notes | Document physician presence |
Incorrect modifier use | Review modifier requirements |
Bundling violations | Check CCI edits |
Insufficient documentation | Include all required elements |
If you’re dealing with billing challenges, you can check out our medical billing consulting services for expert assistance.
Insurance Coverage for CPT 93016
Most insurance plans cover the 93016 CPT Code when medically necessary. Coverage depends on proper documentation and medical indication.
Medicare covers the procedure with specific requirements. Private insurance plans generally follow Medicare guidelines.
Insurance Type | Coverage Details |
Medicare Part B | Covered with medical necessity |
Commercial Insurance | Usually covered |
Medicaid | State-dependent coverage |
Worker’s Compensation | Case-by-case basis |
Reimbursement Rates for CPT 93016
Reimbursement varies by geographic location and insurance type. Medicare sets the baseline rates for most payers.
The national average Medicare rate provides a reference point. Commercial insurance often pays higher rates than Medicare.
Payer Type | Average Reimbursement |
Medicare | $45-65 nationally |
Commercial Insurance | $60-90 typically |
Medicaid | $35-50 average |
Cash Pay | $75-125 range |
For help with revenue cycle optimization, you can check out our revenue cycle management services page.
Related CPT Codes
Several CPT codes relate to cardiovascular stress testing. Understanding these relationships helps with proper billing.
Some codes bundle together while others bill separately. Knowing these rules prevents billing errors.
Related Code | Description | Billing Relationship |
93015 | Complete stress test | Cannot bill together |
93017 | Tracing only | Separate component |
93018 | Interpretation only | Cannot bill with 93016 |
93350 | Stress echocardiography | May bill together |
Common Denial Reasons
Insurance companies deny CPT 93016 claims for several reasons. Understanding these reasons helps prevent future denials.
The most frequent denial involves a lack of medical necessity. Proper documentation addresses this issue.
| Denial Reason | Prevention Strategy |
| Medical necessity | Document clinical indication |
| Missing authorization | Obtain prior approval |
| Duplicate billing | Check previous claims |
| Incomplete documentation | Include all required elements |
For expert help with denial management, you can check out our denial management services to reduce claim rejections.
Best Practices for CPT 93016
Following best practices improves claim acceptance rates. These practices also reduce administrative burden.
Staff training on proper documentation helps avoid common mistakes. Regular audits identify potential problems early.
| Best Practice | Implementation |
| Staff education | Regular training sessions |
| Documentation audits | Monthly record reviews |
| Prior authorization | Verify requirements |
| Clean claim submission | Review before sending |
Quality Measures and Reporting
Healthcare facilities often track quality measures for stress testing. These measures help improve patient care and billing accuracy.
Tracking denial rates identifies billing problems. Regular reporting helps maintain high standards.
| Quality Measure | Target Goal |
Claim acceptance rate | >95% |
Documentation compliance | 100% |
| Prior authorization completion | >98% |
| Patient safety incidents | Zero tolerance |
For detailed reporting and analytics, you can check out our medical billing reporting solutions page.
Compliance Considerations
HIPAA compliance remains essential for all medical billing activities. Patient privacy protection applies to all billing processes.
Audit trails document all billing activities. These records help during insurance reviews and compliance audits.
| Compliance Area | Requirements |
| HIPAA Privacy | Patient information protection |
| Audit documentation | Complete record maintenance |
| Staff training | Regular compliance education |
| Security measures | Data protection protocols |
For complete HIPAA compliance support, you can check out our HIPAA compliance services page.
Technology Integration
Modern EHR systems help with CPT 93016 billing. These systems automate many billing processes and reduce errors.
Integration with billing software improves efficiency. Automated coding suggestions help reduce mistakes.
| Technology Feature | Benefit |
| Automated coding | Reduces manual errors |
| Documentation templates | Improves completeness |
| Real-time eligibility | Prevents coverage issues |
| Electronic claims | Faster processing |
Training and Education
Staff education improves billing accuracy for CPT 93016. Regular training updates keep teams current with changes.
Certification programs provide advanced knowledge. These programs help staff handle complex billing situations.
If you need help with mental health billing, you can check out our articles about F90.0 ICD-10 code and F11.20 ICD code for additional guidance.
Conclusion
93016 CPT Code requires careful attention to documentation and billing practices. Proper supervision and complete records ensure claim acceptance.
Healthcare providers benefit from professional billing support. Expert assistance reduces denials and improves cash flow. For complete medical billing support, you can visit our main medical billing services page or explore our patient payment services for better collection strategies.